Too many solutions, not enough time (or money)
Employers today have plenty on their plate, yet rising healthcare costs continue to top their list. In response, the market has flooded with point solutions that strive to be the silver bullet for health ailments, health management, member engagement and cost reduction. It’s good business, with half of the nation’s employers contracting with four to nine point solutions, but it means even more work for human resource leaders, who are left to contend with a dizzying amount of vendor vetting, performance analysis and ongoing management. That work doesn’t come cheap. One study found that the direct cost of employers sorting through the complexities of health and benefits administration was approximately $21.57 billion.
Workers don’t have it much easier. Already responsible for managing their own complex health needs in today’s healthcare system, they’re forced to navigate a siloed medical landscape littered with point solutions—a frustrating experience that can feel like a full-time job in itself.
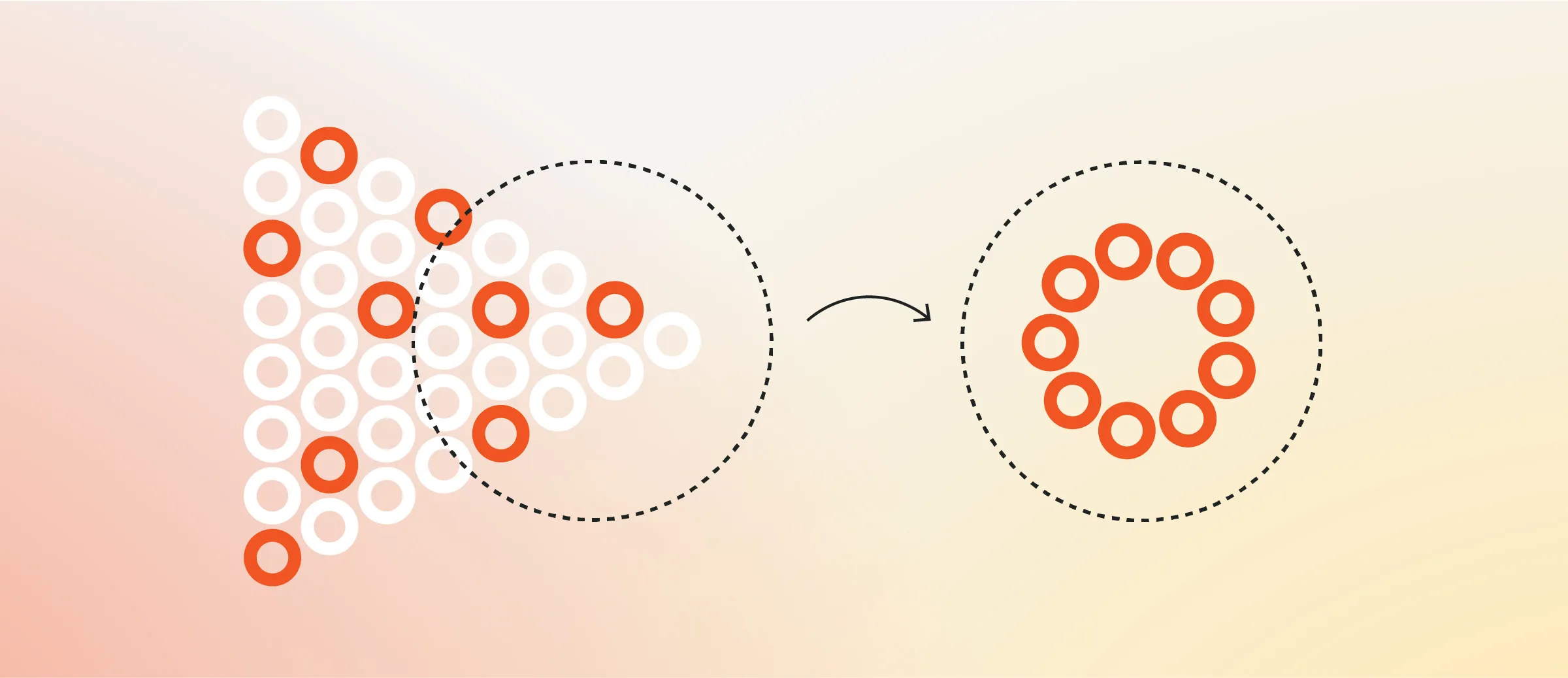
It’s been clear for some time that a solution for employers would be by integrating point solutions and other healthcare touchpoints into a single, cohesive system. But while it might make for an easy buzzword, the truth is that real integration—which requires the meticulous coordination and alignment of countless parties—has proven elusive.
Making integration a reality
Skai Blue Cross Blue Shield’s health solution Celeste makes integration a reality and allows employers and members to get the most out of their point solutions. Through a three-step process, Celeste solves the problem of integration where other approaches have failed.
1. Break through the clutter
While it’s great to have choices, an overwhelming number of employers want or need help understanding and narrowing down the vast array of point solutions available to them. A carefully chosen selection of high-quality point solutions is like a wardrobe that’s been hand-curated by a personal shopper: everything you need, nothing you don’t and none of your precious time lost in the search. That’s why our Market Solutions team has vetted more than 300 solutions across multiple clinical categories to provide a curated, comprehensive hub to meet every employer’s needs.
2. Streamline the process
The more point solutions an employer decides to offer, the more work for them on the backend. Instead of dealing with multiple vendors, Celeste manages everything on the employer’s behalf, increasing point solution effectiveness for employers and members alike, unburdening employers of a huge, expensive and time-consuming administrative responsibility.
3. Optimize member engagement
While individual point solutions are often developed and touted as though they exist in a vacuum, the truth is that they’re only one of many health benefits that an employee has access to. Moving between them can be a chore at best; at worst, it never even happens. That’s why Celeste brings it all together with a frontline team of Care Advocates who can help guide members toward the correct benefit at the correct time—point solution or otherwise—in the context of their healthcare plan more broadly. Or, if members prefer, they can manage these point solutions themselves through the Celeste with Accolade app, an intuitive hub and “single front door” that brings their benefits all together in one place.
Who benefits? Everyone.
While point solutions continue to provide innovative remedies to healthcare challenges, cashing in on their full potential is difficult for employers and members alike.
Having a partner who can remove decision fatigue, provide an integrated hub of highly curated options, deliver tailored consultation, ensure optimal engagement and make the administrative process easy is extremely powerful for employers. Not only does it free up time, but it also leads to better point solution ROI.
For members, having convenient health solutions that cover their spectrum of needs and help them navigate and utilize their benefits to the fullest has a substantial impact on their experience and their health outcomes.
To learn more about Celeste, visit MeetCeleste.com.